ArthritisVitalite Medical Centre2019-12-05T18:29:42+04:00The term arthritis literally means inflammation of the joints and can affect any synovial joint in the body.
In broad terms, there are two types of arthritis namely osteoarthritis and rheumatoid arthritis.
Osteoarthritis
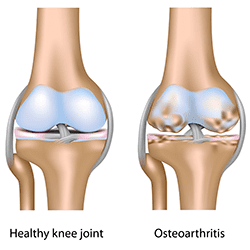
Osteoarthritis is due to normal stress and strains of everyday activity. It is the normal wear and tear of use and is usually age and activity related. The bone is continually in a cycle of building up and breaking down the joint surfaces. As we get older the body builds up the bone less uniformly and can put excess bone in places of stress. This leads to a rough joint surface that can cause pain and inflammation.
Rheumatoid arthritis
Rheumatoid arthritis is part of a family of similar diseases called auto-immune diseases. This occurs when the immune system causes repeated inflammation and over a period of time this can cause the damage to the joint surface. Symptoms can include stiffness, swollen joints, fatigue and joint aches.
There are a variety of different inflammatory arthritis, but the following are the some of the other inflammatory arthritis conditions most commonly seen:
Fibromyalgia
Often called a soft tissue rheumatism as it affects the muscular system and not the joints. It is associated with widespread muscular pain and generalized fatigue and is more common in women. On examination there are active tender points in the muscles that are causing the pain and can be found in a characteristic pattern around the body.
Systemic Lupus Erythemaosus(SLE)
This is a chronic rheumatic disease that affects many parts of the body including joints, muscles, skin, heart, lungs, kidneys and eyes. The cause of Lupus is unknown.
Spondylarthropathy
A collection of diseases fall into this group including ankylosing spondylitis, psoriatic arthritis and Chrohn’s disease. The most common type is ankylosing spondylitis which produces pain and inflammation in the lower back (the sacroiliac joint) is more common in males than females.
Diagnosis
Early diagnosis is important in the management of arthritis. This will involve completing a full medical history of symptoms and a physical examination of the joints. Blood and other laboratory tests are also useful in determining the cause of certain conditions, but may not detect all arthritis problems. X-ray investigation may be required and will show any joint deterioration that is seen in osteoarthritis and later stages of rheumatoid arthritis.
Treatment
Treatment for arthritis can be very effective and requires a team approach. Your rheumatologist will put a plan that is appropriate for your condition and which will generally include medications, regular follow up and testing, and physiotherapy.
Physiotherapy
Your physiotherapist can help you with the management of arthritis in a number of ways. The first involves treatment of symptoms such as joint pain, stiffness and swelling during times of flare up.
Soft tissue massage, joint mobilization and
electrotherapy are used at this stage as well as splinting and strapping to support the joint.
Once the joint is more stable and the episode of flare up has passed, prevention and management of future episodes is important. Your physiotherapist will guide you through and advice on appropriate exercises that should be done to strengthen muscles supporting the joints and to maintain range of motion.
Arthritis need not be a condition to be feared. With early detection and management, both medical and physiotherapeutic, the disease can be managed completely. There is no need to be living in pain or fearing joint deformity and you can lead an active healthy lifestyle.